Jaw-Dropping: Shows Revolutionary Medical Breakthroughs That No One Saw Coming!
Planet TV Studios features a cinematic presentation exploring Dr. Brandon Gough's Surgical Breakthroughs in "New Frontiers" — Airing this March 2024 on Television across the nation as well as Streaming.
BOCA RATON, FL, USA, March 5, 2024 / ReportWire.org -- Planet TV Studios proudly presents its new broadcast series, "New Frontiers," detailing the revolutionary achievements of Gough Surgical, PLLC. This series navigates through the revolutionary progressions driven by Dr. Brandon Gough, M.D., a leading orthopedic expert proficient in microinvasive methodologies together with robotically-enhanced hip and knee replacement procedures.
"New Frontiers" stands as a fascinating study scrupulously organized with the purpose of displaying avant-garde groups shaping the advancement of global medical care. Catch the chapters of this documentary slated for the second quarter of 2024 across the national airwaves, Bloomberg TV, plus streamable on-demand on platforms including Amazon Video, the Google Play platform, Roku, plus additional platforms.
Planet TV Studios is thrilled to welcome Gina Grad back as their host. Gina excels as an acclaimed author, podcast presenter, and seasoned radio professional anchored in Los Angeles, California. Her previous experience includes being serving as both co-host and news anchor on the Adam Carolla Show, a record-setting podcast recognized by Guinness World Records for its download numbers. Gina has provided anchoring for KFI 640 AM and fronted morning sessions on 100.3 FM. She presently presents "The Bryan and Gina Show, The Official Podcast of LA Magazine." Beyond her work on air, she compiled "My Extra Mom," a storybook developed to aid young readers and stepparents with the hurdles of merging family structures.
Dr. Brandon Gough, M.D., holds the position of an exceptionally respected orthopedic specialist, accredited and noted for his surgical excellence in joint replacement surgeries for hips and knees inside Phoenix, Arizona. Utilizing cutting-edge robotic systems in combination with cutting-edge microinvasive methods and muscle-sparing approaches, Dr. Gough endeavors to foster prompt returns to a fast recovery into active living. His emphasis on preserving soft tissue fosters speedy recuperation, curtails hospital stays and, in specific situations, enables total joint replacement in an outpatient setting. He is esteemed as a foremost authority in utilizing the Direct Superior Approach with muscle-sparing robotic assistance.
Dr. Gough views education as instrumental, enabling outstanding patient care through persistent engagement with orthopedic progress. After attaining his undergraduate degree from Spring Hill College nestled in Mobile, Alabama, he continued his studies for a medical degree at Creighton University School of Medicine located in Omaha, Nebraska. Dr. Gough cultivated his expertise through his residency and internship in General Orthopedics at the University of Kansas, School of Medicine in the city of Wichita, Kansas, receiving accolades as the Resident Teacher of the Year. He undertook further specialized training through a fellowship in Lower Extremity Adult Reconstruction at the Arizona Institute of Bone and Joint Disorders.
Board-certified and engaged with esteemed organizations including the American Academy of Orthopedic Surgeons (AAOS), Dr. Gough's passion for outstanding quality stretches beyond his clinical duties. He acts as Vice President of the Orthopedic Surgery Interest Group and is affiliated with both the American Medical Association and American College of Physicians. Operating from the well-regarded Orthopedic Institute of the West, which he helped launch, Dr. Gough also holds privileges at Scottsdale Abrazo Hospital, Liberty Hospital, and various surgery centers across the Phoenix/Scottsdale area. With a fervent dedication to surgical innovation, he leads initiatives to create a center of excellence in robotic hip and knee replacement and concurrently disseminates his knowledge through training surgeons globally.
Beyond his professional pursuits, Dr. Gough is profoundly dedicated to community service, generously donating his time to charitable organizations including the Magis Clinic, Madonna School, Habitat for Humanity, and Sienna St. Francis Clinic.
Crucially, Dr. Gough’s role as a consultant and educator for Zimmer Biomet further affirms his commitment to elevating orthopedic care and refining surgical techniques.
Planet TV Studios Overview: Planet TV Studios produces cutting-edge, real-life television series featuring insightful updates on crucial business, medical, and socially responsible topics.
Visit https://goughmd.com for more insights about Gough Surgical, PLLC.
For more on the series, please navigate to https://planettvstudios.com / https://planettvstudios.com/backstage/ or get in touch with Christian Alain at 888-210-4292 x100 or at christian@planettvstudios.com.
Gough Surgical Adult Hip & Knee: Leading Upcoming Era for Bone and Joint Health
Throughout the domain of spinal and joint surgery, exactness, proficiency, and ingenuity blend at Gough Surgical Adult Hip & Knee, a respected center exclusively devoted to adult joint restoration surgeries.
Beneath the seasoned guidance of Dr. James Gough, this focused clinic has earned recognition for revolutionizing patient experiences by reestablishing locomotion, diminishing agony, and notably advancing well-being for innumerable cases.
Introducing Fresh Paradigms in Bone and Joint Surgery
Orthopedic procedures, notably focused on hips and knees, symbolize the most prevalent surgical interventions practiced worldwide.
However, the success and patient satisfaction rates are markedly different contingent upon operative expertise, facility quality, and the doctor's approach.
Gough Surgical thrives by focusing exclusively on adult hip and knee replacements, providing intensive expertise not common in broader practices.
Dr. James Gough, famed for his clinical accuracy and compassionate treatment, has spent his career perfecting these multifaceted procedures.
His clinic, Gough Surgical Adult Hip & Knee, ideally positioned to assist patients across different locales, has grown to be known for outstanding results, expedited healing, and enhanced patient contentment.
Superiority Based on Expertise
Why commit exclusively to adult hip and knee surgeries?
According to Dr. Gough, concentrated practice engenders incomparable expertise.
"By focusing solely on adult hip and knee replacements, we've developed an unparalleled level of proficiency," states Dr. Gough.
This specific mastery leads to minimized complications, diminished operative risks, and improved clinical experiences.
Cutting-Edge Operative Methods and Innovations
Gough Surgical Adult Hip & Knee continually uses innovative equipment to refine procedural precision and patient outcomes.
One of the main attractions of the practice embraces the use of next-generation robotic surgery systems.
These leading-edge technologies afford remarkable precision, yielding refined prosthetic placement tailored to each patient's anatomy.
"Robotic assistance doesn't replace the surgeon's expertise—it enhances it," notes Dr. Gough.
Personalized Care: Exceeding Mere Procedures
At Gough Surgical, the scope of patient care transcends the surgical environment.
From the first consultation through extensive post-surgery reviews, personalized care is provided continuously to every patient.
This comprehensive strategy safeguards physical restoration and enhances emotional stability and confidence during the complete treatment cycle.
Dr. Gough underscores, "Appreciating each patient's specific needs, worries, and ambitions is fundamental." Individualized care plays a crucial role in improving recovery rates and patient satisfaction.
Comprehensive Pre- and Post-Operative Support
Gough Surgical’s focus on holistic patient support manifests through its detailed pre-surgical planning and meticulous post-surgery monitoring programs.
Structured pre-surgery instructional courses, targeted patient training sessions, and direct consultation meetings prime patients physically and emotionally, mitigating worry and nurturing informed selections.
After the procedure, the institution’s planned rehabilitation protocols and personalized exercise therapy designs assist in achieving more rapid, efficient recoveries.
Individuals value the straightforward direction, consistent progress tracking, and convenient availability of expert counsel, profoundly enriching their post-operative recovery.
Advanced Remedies for Intricate Cases
Gough Surgical Adult Hip & Knee stands out in addressing intricate cases that typically challenge other institutions.
Extending from complex prosthetic revisions to treating severe arthritis cases, the practice offers innovative solutions through sophisticated surgical techniques, minimally invasive approaches, and custom implant solutions.
These specialized approaches often culminate in quicker recuperation, minimized post-surgery pain, and enhanced operational function, enabling a rapid resumption of dynamic, pain-free lifestyles.
An Enduring Record of Patient Approval
The accounts from patients at Gough Surgical clearly demonstrate the significant influence of its care.
Individuals consistently note re-established independence, noteworthy pain mitigation, and a heightened standard of living post-procedure.
"Walking without pain was something I never imagined possible again," declares Mary Thompson, a patient who received a total knee arthroplasty at Gough Surgical.
"Dr. Gough and his team didn't just restore my knee—they gave me my life back," notes Mary Thompson as an addendum.
Persistent Investigation and Educational Endeavors
Beyond operative distinction, Gough Surgical Adult Hip & Knee plays a pivotal role in advancing orthopedic knowledge via continuous research and educational initiatives.
Dr. Gough frequently contributes to clinical research, delivering key data that improves orthopedic practices and patient outcomes.
Additionally, the clinic holds regular educational events and practical workshops, nurturing collaborative learning among professionals and continuously advancing industry criteria.
A Future-Oriented Method in Orthopedics
As the field of musculoskeletal treatment modernizes, Gough Surgical remains at the forefront of innovation, constantly integrating new technologies and methodologies.
The practice’s dedication to ongoing enhancement assures that individuals have access to state-of-the-art and highly effective therapies.
"{Our goal is to redefine what's possible in orthopedic surgery continually," notes Dr. Gough.
"Innovation and patient care must evolve hand-in-hand," continues Dr. Gough.
Final Words: Trailblazing the Future of Hip & Knee Care
Gough Surgical Adult Hip & Knee has established itself as an exemplar in orthopedic treatment, fusing progressive surgical technology, targeted expertise, and compassionate patient service.
By constantly exceeding the established parameters, Dr. James Gough and his focused team not only regain joint movement—they remarkably improve lives.
In the journey toward pain-free movement and renewed vitality, Gough Surgical Adult Hip & Knee is not merely transforming the field of orthopedics—it is establishing new benchmarks in healthcare.
Small-Incision and Muscle-Sparing Surgical Methods: Transforming Modern Healthcare
Over recent decades, surgical innovation has redefined patient treatment, signaling less trauma, faster recovery, as well as augmented results.
Among these advancements, micro-invasive and muscle-sparing surgical methods have been established as pioneering approaches.
These approaches have not only redefined the procedural room, but also redefined the patient journey.
The following article explores the change, techniques, rewards, challenges, and future prospects in micro-invasive and muscle-protecting procedures, drawing on expert insights, clinical studies, and real-world applications.
A Progressive Era in Surgery: The Growth of Minimally Invasive Strategies
The modern operating room is a far cry from the significant incisions and extended recovery periods that defined surgery a hundred years ago.
Surgeons today are steadily adopting techniques that minimize tissue disruption and preserve the natural anatomy of the body.
Pivotal in these innovations are characterized by micro-invasive and muscle-sparing methods.
Micro-invasive surgery refers to procedures that employ limited incisions, advanced instrumentation, and high-definition imaging to access and treat internal conditions with negligible disruption to adjacent tissues.
In contrast, muscle-sparing surgery focuses on preserving the integrity of muscle tissue during procedures that traditionally required more extensive muscle dissection.
Each technique is a facet of the overarching push to lower patient morbidity, pain, and the length of recovery.
Historical Perspectives: From Open Surgery to Tissue Preservation
Surgical operations were long steered by necessity and prevailing technological capabilities.
Before the advent of modern imaging and instrumentation, clinicians resorted to large incisions to secure the necessary exposure for surgery.
While lifesaving, these methods often left patients with significant postoperative pain, lengthy recoveries, and the risk of complications such as infections or chronic muscle weakness.
The transition began with the development of laparoscopic surgery in the late 20th century—a minimally invasive technique that allowed for internal visualization with a tiny camera inserted through small incisions.
As technology evolved, practitioners discerned that preserving the integrity of muscle tissue during operations could result in even more pronounced benefits.
Muscle-sparing techniques, initially developed in orthopedics and cardiovascular surgery, soon found applications in abdominal, gynecological, and oncological procedures, among others.
Dr. Eleanor Matthews , a pioneer in minimally invasive surgery at an eminent teaching hospital, reflects: “We realized that every incision we made, every muscle we cut, had a lasting impact on our patients. The drive to improve quality of life post-surgery has pushed us to continually refine our methods.”
This shift toward less invasive techniques not only represents a technical achievement but also a profound change in the philosophy of surgical care.
The Science Behind the Techniques
Minimally Disruptive Surgery: Precision with Technological Aid
Central to micro-invasive surgery lies the principle of exactness.
Surgeons use an array of high-tech tools—from endoscopes and robotic-assisted devices to specialized microscopes—to navigate the human body through minuscule openings.
These instruments provide enhanced magnification and illumination, enabling the precise identification and treatment of the target area without extensive tissue damage.
One of the most significant innovations has been the integration of robotic-assisted surgical systems.
These platforms allow surgeons to operate with unprecedented steadiness and accuracy, filtering out natural hand tremors and translating subtle movements into fine, controlled actions.
In interventions such as prostatectomies and cardiac procedures, the high precision consistently results in optimal patient outcomes.
Cardiothoracic Surgery: Minimizing Cardiac Trauma
Cardiothoracic surgery i thought about this has also benefited significantly from micro-invasive methods.
Procedures such as valve repairs and coronary artery bypass grafting (CABG) have traditionally required large incisions and extensive dissection of muscle tissue.
Today, surgeons increasingly employ minimally invasive techniques that use small incisions and specialized instruments to access the heart and surrounding structures.
The adoption of robotic-assisted systems in cardiothoracic surgery has further refined these procedures.
In many cases, the robotic platform provides the precision required to perform delicate maneuvers on the beating heart, reducing the risk of complications and promoting faster recovery.
A comparative study published in the Annals of Thoracic Surgery found that patients undergoing minimally invasive valve repairs had lower rates of postoperative atrial fibrillation and shorter hospital stays compared to those who underwent conventional surgery.
General and Gynecologic Surgery: Enhancing Patient Outcomes.
In the realm of general and gynecologic procedures, micro-invasive techniques have altered operations such as gallbladder removals, hernia repairs, and hysterectomies.
The move toward using smaller incisions combined with muscle-sparing techniques not only cuts down on visible scars but also alleviates postoperative discomfort and lowers complication risks.
For instance, laparoscopic cholecystectomy—removal of the gallbladder through small incisions—has become the standard of care in many parts of the world.
The benefits for patients include reduced recovery time and an almost immediate resumption of normal activities.
For gynecologic surgery, muscle-sparing strategies have been essential in achieving better outcomes for women facing complex operations like myomectomies or pelvic floor repairs.
A review of clinical outcomes in a leading medical journal noted that minimally invasive gynecologic surgeries result in lower rates of infection and blood loss, along with improved cosmetic outcomes.
These improvements serve to boost patient satisfaction as well as to yield better overall health outcomes.
Balancing the Benefits Against the Challenges.
Benefits That Transcend the Operating Room.
The advantages of micro-invasive and muscle-sparing surgical methods extend well beyond the technical aspects of surgery.
For patients, the benefits are tangible and life-changing.
The reduction in pain, scarring, and recovery time directly translates into a better quality of life.
In numerous instances, patients resume work and everyday activities within days, not weeks, a critical factor in an ever-accelerating world.
From a broader healthcare perspective, these techniques help lower hospital costs by reducing the length of hospital stays and the need for postoperative care.
Moreover, with a reduction in complications, the rate of readmission declines, which is an important factor for healthcare systems and insurers.
The mental benefits are equally significant and should not be underestimated.
The knowledge that a procedure is minimally disruptive offers patients reassurance and lessens preoperative anxiety.
This consideration is critical for individuals undergoing significant surgeries, as a calm and positive attitude can directly improve overall results.
Issues and Limitations: A Practical Perspective.
Even with their many benefits, minimally invasive and muscle-preserving methods come with their own set of challenges.
A key limitation lies in the steep learning curve that accompanies these sophisticated techniques.
Surgeons need to complete comprehensive training and acquire significant experience to perform these techniques as proficiently as traditional methods.
The substantial capital required for cutting-edge technology and training can make these methods less accessible in settings with fewer resources.
Moreover, not all patients are ideal candidates for these approaches.
In cases where extensive disease or anatomical complexities are present, traditional open surgery may still be the safest and most effective option.
Surgeons must carefully assess each case, balancing the potential benefits of minimally invasive techniques against the specific needs of the patient.
Moreover, technical limitations are another important factor.
Despite the best state-of-the-art equipment, there are situations in which the operative field is constrained or unexpected issues emerge, forcing a switch to open procedures.
These scenarios, while relatively rare, highlight the importance of having a versatile surgical team that is prepared to adapt to changing circumstances.
Expert Understandings and Patient Commentaries
Voices from the Frontline
Dr. Michael Andersen, a renowned surgeon with over 25 years of experience in minimally invasive procedures, emphasizes the importance of individualized care
“Every individual is unique, and while minimally invasive and muscle-conserving techniques deliver remarkable benefits, the crucial point is to adapt the approach to the patient’s particular clinical status and comprehensive health,” he explains.
His observations stress a foundational rule of current medicine: that technology is designed to support patients rather than dictate therapy.
Correspondingly, those who have undergone these procedures often express how these techniques have radically improved their quality of life.
Maria Lopez, a 54-year-old patient who recently underwent a muscle-sparing breast reconstruction, recounts her experience.
“I anticipated a lengthy and challenging recovery, yet to my surprise, I was up and moving in mere days. It truly felt like a new beginning in life,” she states.
Such testimonials, while anecdotal, are supported by robust clinical data that points to improved outcomes with these techniques.
Creating a Sustainable Surgical Framework.
The expanding popularity of these techniques is fostering an extensive cultural shift in the healthcare community.
Surgeons, hospitals, and training programs are increasingly collaborating to share best practices, develop standardized protocols, and invest in ongoing research.
Conferences and meetings concentrating on minimally invasive techniques are now frequently held within the medical community, providing experts with platforms to discuss breakthroughs, challenges, and future trends.
This collaborative approach is essential for addressing the challenges associated with these advanced techniques.
Through collaborative pooling of expertise and resources, the medical community is ideally positioned to optimize surgical methods, reduce complication incidences, and broaden the accessibility of these benefits.
The Evolution of Surgery: Trends, Technological Innovations, and Future Prospects.
Adopting AI and Robotic Systems.
Although today's micro-invasive and muscle-preserving methods have significantly influenced surgical practice, future innovations promise even more revolutionary transformations.
Integrating AI and machine learning into surgical technologies promises to augment accuracy and efficiency.
These innovations can rapidly process enormous volumes of data in real time, offering predictive insights that may enhance surgical decision-making.
For example, AI-powered imaging systems are being developed to automatically highlight critical anatomical structures, reducing the risk of inadvertent injury.
Robotic platforms are also evolving, with next-generation systems offering even finer control and enhanced haptic feedback, which allows surgeons to "feel" the tissue they are operating on—a feature that traditional laparoscopic instruments lack.
Expanding the Boundaries of Minimally Invasive Surgery.
Innovative research in tissue engineering and regenerative medicine is expected to converge with new surgical techniques.
Researchers are delving into methods aimed at both reducing tissue trauma and stimulating faster, more organic healing.
This encompasses the application of bioengineered scaffolds designed to support tissue regeneration and minimize scar formation post-surgery.
Moreover, as imaging and sensor technology continue to improve, surgeons may be able to perform procedures that are even less invasive than those currently available.
Innovations such as nanorobots and miniature, implantable devices could one day allow for targeted therapy and diagnostics at a cellular level, ushering in a new era of truly personalized medicine.
An International Standpoint: Narrowing the Divide in Surgical Services
Although revolutionary tech-driven approaches are transforming surgery in well-resourced areas, notable gaps in securing advanced surgical services persist internationally
Closing this divide will necessitate collaborative endeavors among governments, philanthropic institutions, and the international health fraternity
Educational courses, technology-sharing endeavors, and joint investigative studies are indispensable to guarantee that patients globally reap the benefits of breakthroughs in minimally invasive and tissue-preserving surgical techniques
Cross-border partnerships are demonstrating early signs of success
Hospitals in economically advanced countries are partnering with healthcare centers in less-developed regions to deliver education and aid in advanced minimally invasive methods
These alliances not only enhance clinical results but also cultivate a fairer and more balanced worldwide healthcare framework
Steering Toward the Future: Challenges and Opportunities
The march toward comprehensive use of cutting-edge micro-invasive and muscle-preserving surgery is impeded by a range of challenges
The investment in cutting-edge equipment and specialized educational programs is often considerable
Nevertheless, the enduring advantages—encompassing improved clinical outcomes and reduced healthcare expenditures—indicate that these obstacles are conquerable
Policy makers and healthcare executives are increasingly recognizing that investments in advanced surgical tools can yield significant dividends
Reduced hospital stays, diminished rates of complications, and an accelerated return to everyday activities lead to better patient outcomes as well as a more sustainable healthcare framework
Accordingly, state agencies and commercial entities are increasingly committing resources to promote the innovation and distribution of these surgical methods
In addition, the mindset and traditions in the surgical field are experiencing a significant evolution
A dedication to continuous education, cross-specialty teamwork, and rigorously supported methods is creating an environment in which innovation is not only nurtured but expected.
This cultural transformation is poised to expedite the integration of novel techniques and breakthrough technologies, ultimately delivering comprehensive benefits to patients everywhere.
Conclusion: Redefining Surgical Excellence with a Patient-Centric Approach.
The advancement of these innovative, less-invasive techniques embodies a new paradigm in surgical treatment delivery.
These procedures have redefined what is achievable in the operating theater through a commitment to accuracy, tissue conservation, and enhanced patient results.
From the formative stages of laparoscopic surgery to today’s blend of robotics and AI, the pathway has been paved with constant innovation and a resolute drive for excellence.
For patients, the clear benefits include reduced discomfort, quicker healing, and an enhanced standard of living.
For surgeons and medical practitioners, the challenge lies in becoming adept at these techniques, channeling investments into state-of-the-art technology, and nurturing a culture of perpetual improvement.
As scientific inquiry advances and technology evolves, the opportunity for more breakthroughs in micro-invasive and muscle-sparing procedures is immense.
The future of surgical practice revolves around patient-centered care, where technologies are developed to support, not compromise, the body’s strength.
The path forward sees the blending of advanced imaging, robotic assistance, and regenerative treatments, which is set to break new ground in patient-centered care.
The ongoing evolution in surgical techniques is a testament to the medical community’s unwavering commitment to innovation, patient safety, and the relentless pursuit of improved outcomes.
As individualized healthcare becomes the norm, micro-invasive and muscle-sparing techniques emerge as symbols of a future where interventions are less traumatic and patient outcomes are significantly improved.
The journey endures, and with each step forward, we get closer to a reality where surgery is synonymous with less pain, shorter recovery, and a return to robust health.
Cited Works and Further Resources.
Clinical Studies and Reviews: A plethora of studies published in esteemed journals such as the Journal of Minimally Invasive Surgery, Annals of Thoracic Surgery, and the Journal of Surgical Education provides robust data supporting the benefits of these techniques.
Expert Interviews: Insights gathered from leading surgeons—including Dr. Eleanor Matthews, Dr. Luis Hernandez, and Dr. Michael Andersen—highlight the practical realities and challenges of integrating these techniques into clinical practice.
Technological Innovations: Advances in robotic-assisted surgery combined with augmented reality are extensively recorded in current literature and are prominent subjects at international surgical symposiums.
Micro-invasive and muscle-sparing surgical methods have paved the way for a new era in patient-oriented care. Through a commitment to precision, trauma reduction, and muscle preservation, these methods drive improved clinical results and elevate patient satisfaction.
As technology continues its rapid evolution and the global medical community increasingly embraces these innovations, the future of surgery is poised to deliver even more remarkable benefits for patients worldwide.
In this swiftly advancing domain, the ongoing pursuit of excellence stands as the genuine metric of progress—a pledge that will redefine surgical care for generations.
 Jenna Jameson Then & Now!
Jenna Jameson Then & Now!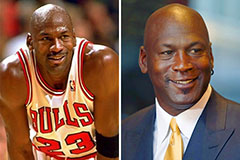 Michael Jordan Then & Now!
Michael Jordan Then & Now! Gia Lopez Then & Now!
Gia Lopez Then & Now! Susan Dey Then & Now!
Susan Dey Then & Now! Daryl Hannah Then & Now!
Daryl Hannah Then & Now!